Paramedic Treatment of Pulmonary Embolism
November 7th, 2013Any patient who presents with signs and symptoms of a pulmonary embolism should be treated as a medical emergency. As pulmonary embolisms rarely present with a clear clinical picture, paramedics must maintain a high index of suspicion with any patient who presents with shortness of breath without a clear clinical cause.
A pulmonary embolism is often caused by the formation of a deep vein thrombosis (DVT) which then breaks free and travels to the lung, causing a blockage within the pulmonary artery. Depending on the size of the thrombus, and the location within the pulmonary arterial tree, this blockage will result in a minor decrease in oxygenation of the blood through to a complete obstruction resulting in sudden death.
It is not uncommon to treat a patient who appears to have a minor respiratory problem, who on further investigations is determined to have a pulmonary embolism. Not all pulmonary embolisms are fatal, but they should all be treated with urgency.
Treatment of a pulmonary embolism first starts with identifying the possibility that a patient has one.
Signs of a Pulmonary Embolism
The following are signs of a pulmonary embolism that paramedics should be aware of:
1. Sudden increase in shortness of breath.
2. Chest pain, particularly pin pointed chest pain. Cardiac chest pain is often difficult for a patient to describe. They will often complain of a heaviness or a funny feeling over the entire chest, where as a person who has a pulmonary embolism will normally describe a sharp pain at the point of the blockage. This makes it particularly difficult for the assessing paramedic, because it is often initially identified as pleuretic pain.
3. Pain or swelling to the calf muscle.
4. Increase respiratory rate without clear clinical causes, such as asthma, COPD, CCF. Be cautious with the patient who appears to be simply hyperventilating, but denies any recent cause of anxiety in an otherwise healthy person.
5. Severely decreased oxygen saturations in a person who has clear breath sounds.
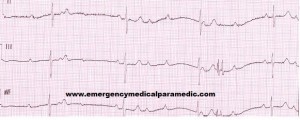
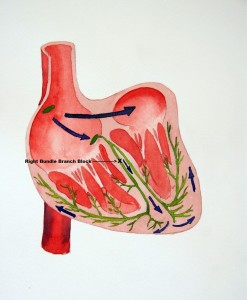
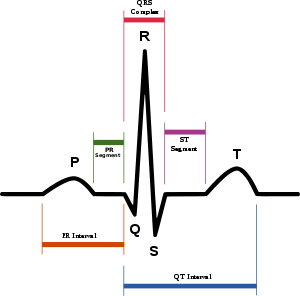
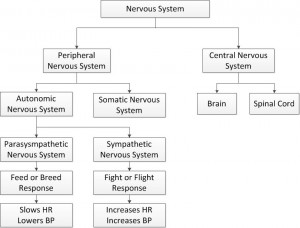
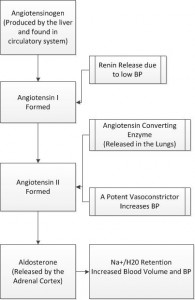
6. Tachycardia, as a means of compensation.
7. S3 and S4 gallop.
8. Cough.
9. Hymoptysis
10. Lower extremity oedema.
Associated conditions that may be the result of a pulmonary embolism or a sign of a pulmonary embolism. These can be applied to a variety of our otherwise well patients!
1. Seizures.
2. Fever – surprising a lot of patients with a pulmonary embolism have a increased body temperature.
3. Abdominal pain.
4. Flank pain.
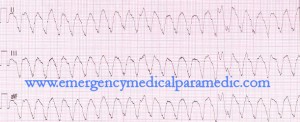
5. New onset of atrial fibrillation.
6. Syncope.
7. Delirium.
Remember, unless you look for it, you will miss it!
Pulmonary Embolism Key Points in History
Because the signs of a pulmonary embolism are so varied it is most commonly picked up by taking a thorough history. The following are vital signs a paramedic should consider when taking a history of any patient who has shortness of breath or chest pain, with an unexplained cause:
1. Recent travel – a study in 2012 identified as little as 4 hours travel within the past month is enough to cause a DVT which then results in a pulmonary embolism.
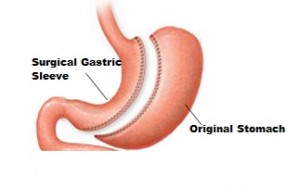
2. Surgery in the past 4 months.
3. Previous diagnosis of a DVT or current diagnosis of a DVT.
4. Recent trauma to the pelvis or lower extremities.
The following are key risk factors that increase the likelihood of a patient getting a pulmonary embolism:
1. Tobacco smoking.
2. Oral contraceptive use.
3. Sedentary lifestyle.
4. Obesity or large calves.
5. Varicose veins.
6. Any known clotting disorders.
7. Chronic obstructive pulmonary disease.
8. Chronic heart failure.
Upon identifying a high likelihood that a patient has a pulmonary embolism a paramedic should focus on urgent transport to a definitive hospital that ideally has cardiothoracic surgical capabilities. The patient should be oxygenated with high flow oxygen if conscious. IV access and early hospital notification should be provided, but not if it will delay the patient getting to hospital. Little research has been completed on pre-hospital use of anticoagulant therapies, but potentially these will come in future years.